Asthma (Adult)
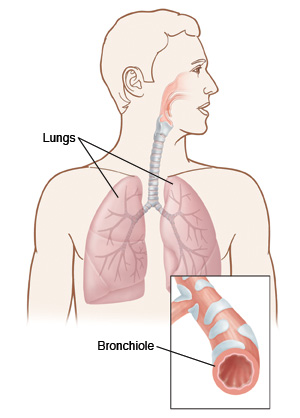
Asthma is a disease in which the medium and small air passages in the lungs go into spasm. This limits air flow. Inflammation and swelling of the airways cause more blockage. During an acute asthma attack, these things cause wheezing, coughing, trouble breathing, and chest tightness.
An asthma attack can be set off by many things. Common triggers include infections, such as the common cold, bronchitis, and pneumonia. Irritants, such as smoke or pollutants in the air, very cold air, strong emotions, and exercise, can also set off an attack. In many adults with asthma, allergies to dust, mold, pollen, and animal dander can cause an asthma attack. Skipping doses of daily asthma medicine can also bring on an asthma attack.
Asthma can be controlled using the correct medicines prescribed by your health care provider. You can also control it by staying away from known triggers including allergens and irritants.
Home care
-
Take prescribed medicine exactly as advised. Ask your health care team for help if you have questions about how to use your inhaler or nebulizer.
-
Call your provider or get medical care right away if you need quick-relief medicine, such as from an inhaler or aerosol breathing machine (nebulizer), more often than prescribed.
-
If you are prescribed an antibiotic or the steroid prednisone, take all of the medicine as prescribed. Keep taking it even if you are feeling better after a few days.
-
Don't smoke. Ask your provider for resources, such as organizations and websites, to help you quit. Stay away from the smoke of others. Don't let anyone smoke in your home, in your car, or around you. And don't use e-cigarettes.
-
Some people with asthma find their symptoms get worse when they take aspirin and nonsteroidal anti-inflammatory drugs or fever-reducing medicines, such as ibuprofen and naproxen. Talk with your provider if you think this may apply to you.
-
Stay away from your asthma triggers.
Follow-up care
Follow up with your health care provider, or as advised. Always bring all of your current medicines to any appointments with your provider. Also bring a complete list of medicines, even those you take for other conditions.
Bring your Asthma Action Plan to all appointments. If you don't have one, talk with your provider about making your own Asthma Action Plan.
Get the COVID-19 vaccine, pneumonia (pneumococcal) vaccine, and yearly flu shot (every fall). Ask your provider about this.
When to get medical care
Contact your health care provider right away if:
-
You have more wheezing or shortness of breath.
-
Your asthma symptoms are waking you up at night.
-
You need to use your quick-relief inhaler more often than normal without relief.
-
You have a fever of 100.4ºF (38ºC) or higher, or as advised by your provider.
-
You cough up lots of dark-colored or bloody sputum (mucus).
-
You have chest pain with each breath.
-
You use a peak flow meter as part of an Asthma Action Plan, and you are still in the yellow zone (50% to 79% of personal best) 15 minutes after using quick-relief inhaler medicine.
Call 911
Call 911 right away if:
-
You have trouble walking or talking because you're short of breath.
-
You use a peak flow meter as part of an Asthma Action Plan, and you are still in the red zone (less than 50% of personal best) 15 minutes after using quick-relief inhaler medicine.
-
Your lips or fingernails turn gray, purple, or blue.
-
You feel faint or lose consciousness.