Exercise-Induced Asthma: How to Care for Your Child
Many kids and teens with asthma get flare-ups when they exercise if their asthma is not well-controlled. Some have asthma symptoms only when they exercise and not at other times.
The health care provider examined your child, asked questions about symptoms, then diagnosed your child with exercise-induced asthma. Sometimes health care providers give families an "asthma action plan," which is a written guide for controlling asthma and treating symptoms right away. The plan includes information about prescription medicines and when to use them. It's important that you and your child understand the asthma action plan, know the signs of a flare-up, and know what to do if a flare-up happens.

-
If symptoms start, your child should slow down the exercising. They may need to stop and take medicine. They shouldn't try to "play through" asthma symptoms, as this can bring on a flare-up.
-
If recommended, your child should take medicine:
-
If the health care provider prescribed a medicine to use every day to ease inflammation and prevent symptoms, use it as directed.
-
Warm-up and cool-down routines before and after practicing or playing can help to reduce symptoms. Have your child work with the coach or trainer to develop a routine that works for them.
-
Remind your child to breathe through the nose and take short rest breaks during exercise.
-
Have your child wear a loosely fitting ski mask or scarf over the nose and mouth when playing or exercising outside in cold weather.
-
If air pollution or pollen are triggers, your child may want to exercise indoors when air quality is poor or pollen counts are high.

Call 911 if your child is struggling to breathe, is too out of breath to walk or talk, or turns blue.

What causes exercise-induced asthma? When we breathe through our noses, air becomes warm and moist on its way to the lungs. But during exercise, we breathe more through our mouths than our noses. This brings cool, dry air directly to the lungs, which can irritate them. Some people with exercise-induced asthma might feel symptoms when the air is warm but polluted or full of pollen. Others might get symptoms when swimming if they are sensitive to chlorine.
How do asthma medicines work? Asthma medicines generally work in two ways:
-
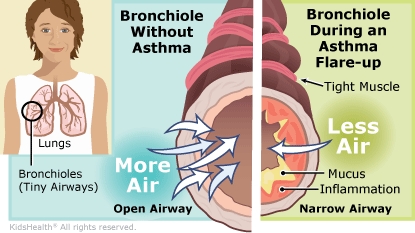
Some asthma medicines work right away to relax the muscles around the airways. This opens the airways and provides quick relief of symptoms. That's why they are sometimes called "quick-relief," "rescue," or "fast-acting" medicines.
-
Other medicines work over time to ease inflammation, which reduces swelling of the airways and limits mucus production. A person usually needs to take these every day, even when they feel fine and have no symptoms. These are sometimes called "controller," "maintenance," or "long-term control" medicines. Some children who have mild asthma might use controller medicines only when their asthma symptoms increase.
Some children will get both types of medicines from one inhaler device. They might need to use this "combination" inhaler every day, with added doses from it when they have symptoms. Some older kids with mild asthma might use a combination inhaler only for quick relief when they have symptoms, or before they exercise. Your health care team will help you figure out which inhaler is best for your child, and how and when to use it.
Can my child still exercise or play sports? Yes. In fact, staying fit and exercising regularly can help to reduce asthma symptoms. It can improve lung function by strengthening the breathing muscles in the chest. So kids and teens with asthma should exercise as much as they can. When asthma is well-controlled, kids with asthma can do anything their peers can do. In fact, many Olympic athletes have exercise-induced asthma, but it doesn't stop them from doing their sport and winning medals.