Caring for Your Child With an Asthma Flare-Up

Asthma flare-ups can be serious. Your child's health care professional will work with you to help prevent flare-ups and keep asthma under control.
There are three types of medicine used at home to treat asthma:
|
Type of Medicine
|
How It Works
|
Generics and Brand Names
|
|
Quick-relief medicines (also called "rescue" or "fast-acting" medicines)
|
Breathed in (inhaled) to relax the muscles in the lungs and open the airways.
|
albuterol – ProAir®, Proventil®, Ventolin®levalbuterol – Xopenex®
|
|
Oral steroids
|
Swallowed, then travel through the body to the lungs to take away swelling during a flare-up. Taken one time or for a few days.
|
prednisone – Deltasone®, Prednicot®prednisolone – Orapred®, Prelone®dexamethasone – Decadron®methylprednisolone – Medrol®, Medrol® Dosepack™
|
|
Long-term control medicines (also called "controller" or "maintenance" medicines)
|
Taken daily to keep swelling away and asthma under control. This is usually a steroid that is inhaled but can be a swallowed medicine.
|
Inhaled:beclomethasone – Qvar®budesonide – Pulmicort®fluticasone – Flovent®fluticasone with salmeterol – Advair®Swallowed:montelukast – Singulair®
|

Many kids have asthma. It is a chronic condition, which means it usually lasts for years, though many kids grow out of it.
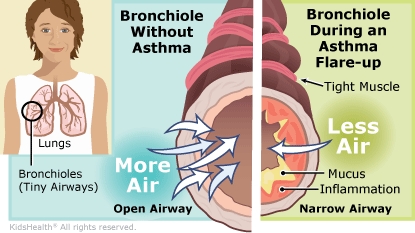
During an asthma flare-up, the muscles in the lungs and airways tighten. The lining of the airways gets swollen and plugged with mucus. This makes it hard to breathe. A child having a flare-up may cough a lot, wheeze, feel chest tightness, or be short of breath. It's important to treat a flare-up as soon as symptoms start.
A trigger is something that can cause asthma symptoms to start. A trigger does not cause asthma.
Examples of triggers include:
Triggers don't bother most people, but they can make people with asthma have a flare-up. Different people with asthma can have different triggers. Some kids outgrow triggers as they get older. Avoiding triggers and taking prescribed medicines are important ways to control asthma.
The health care professional examined your child and asked questions about symptoms. Your child may have been given medicine by mouth or medicine to breathe during the visit to stop the asthma flare-up, or you may have been given a prescription to use at home.
The health care professional reviewed your child's asthma action plan with you and your child. The goal of the plan is to prevent flare-ups and treat a flare-up early. You were taught how to treat symptoms during this and any future flare-ups. It's important that you and your child understand the asthma action plan, know the signs of a flare-up, and know what to do if a flare-up happens.

-
While your child is getting better from this flare-up:
-
When your child's breathing is back to normal:
-
Be sure to follow the asthma action plan.
-
Long-term control medicines should be taken every day as directed, even if your child is feeling fine.
-
Quick-relief medicine should be started at the first signs of a flare-up.
-
Be sure your child always uses a spacer with an inhaler.
-
Make sure your child always carries or has quick-relief medicine available. Talk to the school nurse about keeping some of the medicine at school.
-
Your child should avoid tobacco smoke and any known asthma triggers.
-
If your child has an asthma specialist, be sure to tell him or her about any changes to the medicines that were made today.

-
Schedule a follow-up visit with your child's pediatrician or asthma specialist, as recommended.
-
Some kids use a device called a peak flow meter to check on their asthma as part of their action plan. If your child has one, make sure you understand when and how to use it and what your child's peak flow zones are.
-
If anyone in your home smokes, call 1-800-QUIT-NOW for advice on quitting.
-
Make your home and car smoke-free.

Your child:
-
Needs medicine more often than prescribed.
-
Is not being helped by the quick-relief medicine.
-
Is not getting better from this flare-up.
-
Has another flare-up.
Call 911 if your child is struggling to breathe, is too out of breath to talk or walk, or turns blue. Call 911 if he or she normally uses a peak flow meter and can barely blow into it (red zone).